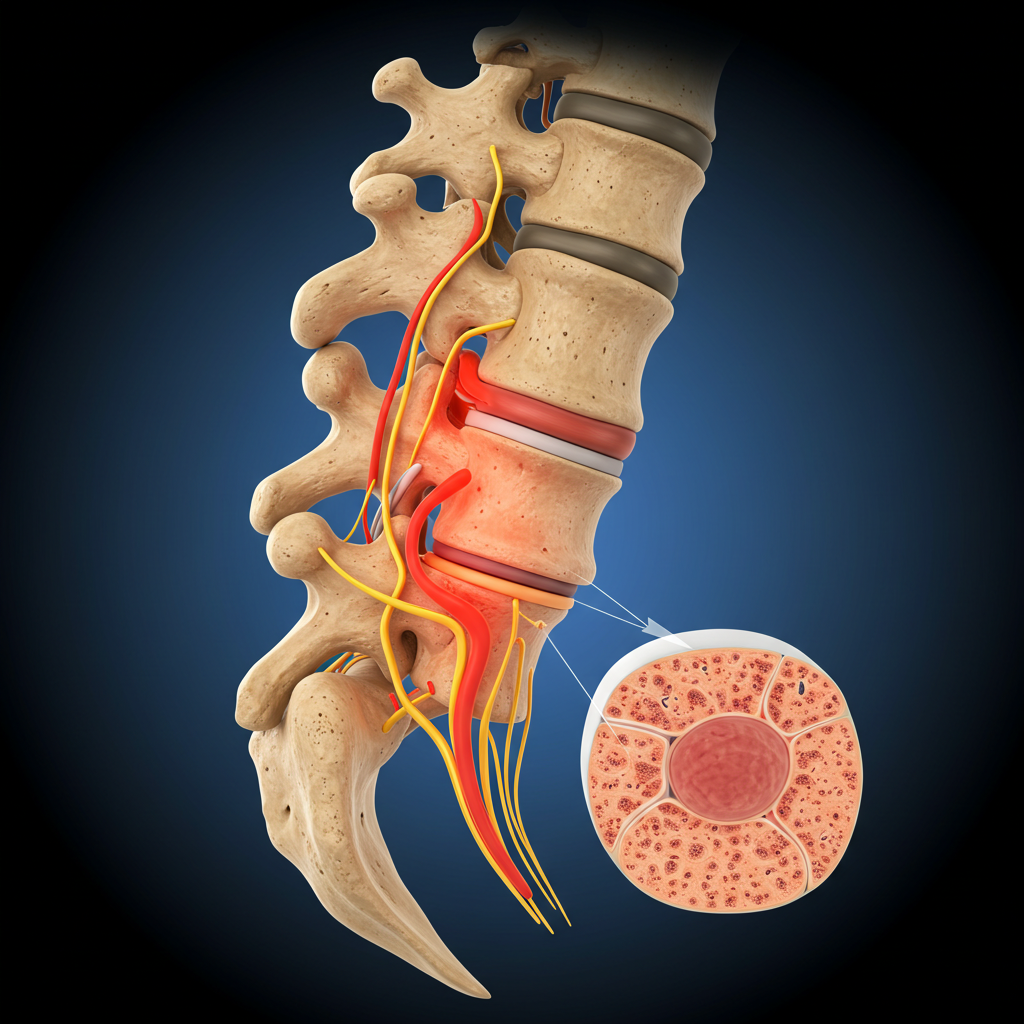
A herniated disc, often called a “slipped” or “ruptured” disc, occurs when the soft, gel-like center of an intervertebral disc pushes through a tear in its tough outer layer (annulus fibrosus). This displacement can irritate nearby nerves, causing pain, numbness, or weakness. It is one of the most common causes of back and neck pain with nerve compression symptoms.
Key Points
Definition & Anatomy
The spine is made up of vertebrae separated by intervertebral discs, which act as cushions and allow flexibility. Each disc has a soft nucleus pulposus inside and a fibrous outer ring (annulus fibrosus). A herniation occurs when the nucleus protrudes through a weakened part of the annulus, potentially compressing spinal nerves or the spinal cord.
Causes and Risk Factors
- Age-related disc degeneration (natural wear and tear)
- Sudden strain, heavy lifting, or twisting motions
- Repetitive stress from poor posture or long sitting
- Trauma or injury to the spine
- Obesity (increased pressure on discs)
- Smoking (reduces blood supply to spinal structures)
- Genetic predisposition to weaker disc structure
Symptoms
- Localized back or neck pain
- Pain radiating to the arms (cervical disc) or legs (lumbar disc)
- Numbness, tingling, or weakness in the affected limbs
- Worsening pain when sitting, coughing, or sneezing
- In severe cases: loss of reflexes or coordination
Red Flags
- Loss of bladder or bowel control (possible cauda equina syndrome)
- Progressive weakness or paralysis in the limbs
- Severe, unrelenting pain unresponsive to medication
- History of cancer, infection, or significant trauma
Diagnosis
Diagnosis begins with a detailed medical history and neurological examination. MRI is the gold standard imaging technique to confirm disc herniation and assess nerve compression. X-rays may help rule out fractures or alignment issues. In some cases, CT scans or electromyography (EMG) can provide additional diagnostic details.
Management & Treatment
1. Conservative (Non-Surgical) Treatment
- Rest and Activity Modification: Avoid activities that worsen pain, but maintain gentle movement.
- NSAIDs: Ibuprofen or naproxen to reduce inflammation and pain.
- Physical Therapy: Exercises to strengthen back and core muscles, improve posture, and relieve pressure on nerves.
- Heat/Ice Therapy: Alternating warm and cold compresses can reduce pain and muscle spasm.
- Epidural Steroid Injections: Used in selected patients to reduce inflammation around affected nerves
2. Surgical Treatment
Surgery is considered when conservative treatment fails after 6–12 weeks or if severe neurological symptoms occur. Common procedures include:
- Microdiscectomy: Removal of the herniated disc fragment pressing on the nerve.
- Laminectomy: Removal of part of the vertebral bone to relieve pressure on the spinal cord.
- Artificial Disc Replacement: Used in selected patients to maintain spinal motion.
Exercise & Rehabilitation
After acute pain subsides, rehabilitation focuses on restoring flexibility, strength, and posture. Regular exercise can prevent recurrence. Recommended exercises include:
- Core stabilization and pelvic tilt exercises
- Gentle stretching of hamstrings and hip flexors
- Low-impact aerobic activities (walking, swimming)
- Postural training and ergonomic correction
Prevention & Lifestyle
- Maintain a healthy weight and stay physically active
- Use proper lifting techniques (bend your knees, keep the back straight)
- Quit smoking to improve spinal health
- Adjust workstation ergonomics for good posture
- Regular stretching and strengthening exercises for core muscles
Prognosis
About 90% of herniated disc cases improve with conservative management. Only a small percentage require surgery, and outcomes are typically excellent. Early movement, education, and posture awareness significantly reduce the risk of recurrence.
References
- Spine.org Clinical Practice Guideline for Lumbar Disc Herniation (2023).
- NICE Guidance: Sciatica and Low Back Pain Management (2024).
- BMJ Best Practice. Herniated Disc and Radiculopathy (2024).
- World Health Organization (2023). Musculoskeletal Health Overview.